Macular Hole
What Is a Macular Hole?
A macular hole is a small break in the macula, the center of the retina which is responsible for your fine, detailed vision. The cells of the macula, known as photoreceptors, convert light into electrical images. The retina then sends these images via the optic nerve to the brain. A healthy macula allows you to do the daily activities you take for granted such as driving, reading, sewing and other detailed work.
Photo Credit: National Eye Institute, National Institutes of Health
When there is a hole in the macula, your vision will be blurry. Although the symptoms may be similar to macular degeneration and most often affects people over age 60, a macular hole is a different eye disorder. If a macular hole exists in one eye, there is a 15-20 percent chance that a macular hole will develop in your other eye.
The vitreous gel is the fluid that fills your eye and is attached to the surface of the retina. As you get older, the vitreous changes shape and begins to shrink, pulling away from the retina. Natural fluids will fill this area, and you may notice an increase in floaters, small flecks that appear in your field of vision. This is normal and for most people, this will not cause a problem.
However, in some cases, the vitreous can tear the retina as it pulls away, causing a macular hole. In addition, some of the fibers in the vitreous can remain on the surface of the retina after it has pulled away. These fibers can contract and the increased tension this creates can also cause a macular hole. In both these situations, the fluid that has replaced the vitreous can leak through the hole and cause a small localized retinal detachment. This is what causes the blurring and distortion of your central vision.
Macular holes can also occur from eye disorders, such as high myopia (nearsightedness), or secondary to a macular pucker (wrinkle) or retinal detachment. Trauma is another cause of macular hole.
Macular holes often begin gradually. In the early stage of a macular hole, you may notice a slight distortion or blurriness in your straight-ahead vision.You may also notice that straight lines begin to look bent or wavy. Reading and performing detailed work with the affected eye may become difficult.
There are four stages to a macular hole:
Stage 1 - Foveal Detachment (Fovea: Center of the macula)
About half of Stage 1 macular holes will progress, while the other half will spontaneously resolve.This is why your retina specialist will want to observe and monitor your vision.
About half of Stage 1 macular holes will progress, while the other half will spontaneously resolve.This is why your retina specialist will want to observe and monitor your vision.
Stage 2 - Full-thickness Holes without Fluid Cuff
Almost all of these holes will progress. For this reason, surgery is usually recommended to preserve your central vision.
Almost all of these holes will progress. For this reason, surgery is usually recommended to preserve your central vision.
Stage 3 - Full-thickness Holes with Fluid Cuff
These holes will usually progress to Stage IV in three to six (3-6) months.
These holes will usually progress to Stage IV in three to six (3-6) months.
Stage 4 - Full-thickness Holes with Vitreous Detachments
Chronic holes greater than 12 months in age usually are not operated on. Although closing the hole is surgically possible, visual recovery is very limited.
Chronic holes greater than 12 months in age usually are not operated on. Although closing the hole is surgically possible, visual recovery is very limited.
The size of the hole and its duration will determine how much it will affect your vision. When a Stage 3 macular hole develops, most central and detailed vision can be lost. If left untreated, a macular hole will cause permanent central vision loss.
Who Is at Risk for a Macular Hole?
As people age, everyone is at risk of developing a macular hole. It is more likely to occur in people over the age of 60. In addition, women are at greater risk than men.
How Is a Macular Hole Detected?
A macular hole is diagnosed during a comprehensive eye examination, which will include:
- Visual acuity test: Testing your vision at various distances
- Dilated eye exam: Examining your retina and the back of your eye
- Tonometry: Measuring your intraocular pressure
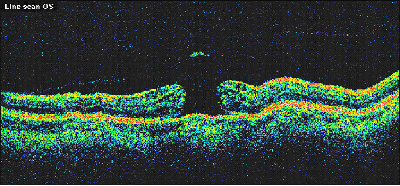
Your doctor may also suggest special tests, called fluorescein angiography or optical coherence tomography (OCT). These tests provide detailed pictures of your retina.
How Is a Macular Hole Treated?
Although some macular holes can seal themselves and require no treatment, surgery is necessary in most cases to help improve vision. In this surgical procedure, called a vitrectomy, the vitreous gel is removed to prevent it from pulling on the retina and replaced with a bubble containing a mixture of air and gas. During the surgery, the internal limiting membrane of the retina is peeled away to relieve tractional forces on the retina that caused the hole to open in the first place. The bubble acts as an internal, temporary bandage that holds the edge of the macular hole in place as it heals. This procedure is performed under local anesthesia by our highly experienced retina specialist. (For more information on retinal operations in our surgery center, please click here.)
Following surgery, most patients must remain in a relative face-down position, normally for one to two weeks. This position allows the bubble to keep the hole sealed. The gas bubble is then gradually reabsorbed by the eye. As the bubble is reabsorbed, your eye’s natural fluids will fill the vitreous cavity. The positioning also helps prevent subsequent cataract formation.
Maintaining a face-down position is usually essential to restoring your vision after surgery. Because this position can be difficult for many people, it is important to discuss this with your doctor before surgery. If you have had an intraocular lens implanted following cataract surgery, maintaining this face down position may not be necessary. In most cases, sleeping prone or on your stomach will be sufficient.
In some instances, if you cannot remain in a face-down position for the required period after surgery, vision recovery may not be successful. If this is the case, you may not be a good candidate for macular hole surgery. However, there are a number of devices that can make the "face-down" recovery period easier on you. There are also some approaches that can decrease the amount of "face-down" time. You should discuss this with your retina specialist.
While performing this procedure, our retina specialist uses 25-gauge transconjunctival sutureless vitrectomy techniques. This method uses the most advanced technology to perform this type of surgery, leading to a more comfortable post-operative course with faster recovery times. (For more information on this procedure, please click here.)
The procedure will be done under local anesthesia, and you will also be given a mild sedative. Your eye will be completely numbed and you will remain comfortable during your surgical experience.
You should not eat or drink anything after midnight the night before your procedure. On the day of treatment, you will be welcomed by a staff member at the surgery center. The staff will help you prepare for your surgery by putting eye drops in your eye. You will be given a gown to wear over your street clothes during your actual surgery.
Because your doctor has inserted a mixture bubble of air and gas to hold the edge of the macular hole in place until it heals, you will not be able to fly and / or to be at high altitude until the gas dissolves, usually over a period of six to eight (6-8) weeks. The air pressure of flying or being at high elevation can cause your eye pressure to rise rapidly and could result in serious complications. You should also avoid having certain types of general anesthesia during this period for another medical condition. Certain gases associated with general anesthesia can also cause similar problems.
After your surgery, you will rest in a comfortable reclining chair. Your family members may then join you in reviewing your follow-up care and schedule. You may be given medication or eyedrops to prevent infection and inflammation. Your surgeon will see you the next day after surgery to check how your eye is healing.
Some mild discomfort is to be expected following surgery. You will wear an eye patch for a short time afterwards. It will take a week for the surface of your eye to fully heal. Depending on the status of your retina, it may take six (6) months or more to attain your final visual result. You may need to avoid strenuous activity while the gas bubble is in place. It will be necessary for you to see your doctor at regular intervals during this time so that he can monitor your healing.
Any surgical procedure involves some risks. The most common risk following macular hole surgery is an increase in the rate of cataract development. In most patients, a cataract can progress rapidly, and often becomes severe enough to require removal. Other less common complications include retinal detachment and infection either during surgery or afterward, both of which must be treated in a timely fashion.
Vision improvement varies from patient to patient. People who have had a macular hole for less than six months have a better chance of recovering vision than those who have had one for a longer period. In most patients, 90 percent of holes can be closed surgically. Discuss vision recovery with your doctor before your surgery. Vision recovery can continue for as long as 6-12 months after surgery.
Because macular holes are a function of aging, as are a number of other age-related disorders including glaucoma and macular degeneration, we recommend annual eye examinations beginning at age 55. Please do your part to protect your vision!
Macular Hole Specialist at Kadrmas Eye Care New England
Meet our ophthalmologist who specializes in the treatment of macular degeneration: