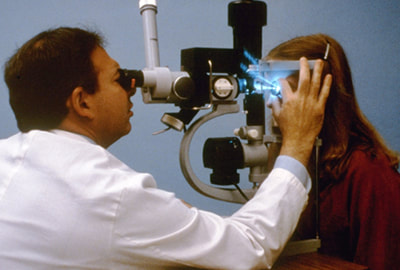
The earlier treatment for glaucoma starts, the better your chances of preventing further damage, which is why it’s so important to be checked for glaucoma early and often if you’re at risk of developing the condition. Treatment for glaucoma may include medication and / or laser or conventional surgery. We’ll discuss each in detail below. Glaucoma MedicationGlaucoma medication usually comes in the form of eye drops. Prescription eye drops prescribed by your ophthalmologist will help to lower the pressure in your eye. Some drops reduce the amount of fluid made, while others promote better fluid drainage. Eye drops for glaucoma can cause side effects, such as stinging, blurred vision, and redness. As the medication in the eye drops is absorbed into the bloodstream, systemic (general) side effects can also develop. The specific side effects depend on the classification of medication used. For example, eye drops containing what are called beta-blockers can cause decreased heart rate, fatigue, and low blood pressure. Your ophthalmologist and pharmacist can discuss the possible side effects associated with your specific glaucoma medication. In some cases, eye drops are not effective in lowering eye pressure, and oral medications may be prescribed instead. Usually, if an oral medication is needed, a classification of drug called carbonic anhydrase inhibitor is prescribed. The oral meds are typically taken two to four times a day. Oral medications tend to cause more side effects than eye drops. Possible side effects are stomach upset, tingling of the fingers, and frequent urination. Again, you can speak with your ophthalmologist and pharmacist about possible side effects you may experience with your medication. To learn more, please visit our webpage, Medical Treatment for Open Angle Glaucoma. Laser Surgery for GlaucomaYour ophthalmologist may also recommend laser surgery to treat your condition if you have glaucoma. The type of laser procedure that you’ll receive will depend upon the type of glaucoma you have. According to the American Academy of Ophthalmology, the two primary laser procedures for glaucoma include trabeculoplasty and iridotomy. A trabeculoplasty is used to treat open-angle glaucoma. The procedure involves focusing a high-energy beam of light on the eye’s drainage system. The laser changes the drainage canal in subtle ways to improve the outflow of aqueous (watery) fluid, which lowers eye pressure. Typically, a laser trabeculoplasty only takes about fifteen minutes. The procedure is usually painless and can be performed on an outpatient basis. It may take a few weeks for eye pressure to decrease and success rates vary. According to the Glaucoma Foundation, a laser trabeculoplasty lowers eye pressure in about 75 percent of the people who have the procedure. The procedure may eliminate the need for eye drops in some people. It can be repeated two or three times in each eye over a lifetime. Another laser procedure for glaucoma is called an iridotomy. An iridotomy is used to treat narrow angle or angle closure glaucoma. The procedure involves using a laser to make a tiny opening in the iris. Creating the small hole diverts the flow of aqueous fluid through the iris to the drainage angle, which reduces eye pressure. To learn more about trabeculoplasty and iridotomy, please visit the following pages on our website: Conventional Glaucoma SurgeryIf medication or laser surgery is ineffective in lowering eye pressure, conventional surgery may be recommended to preserve vision. One of the most common conventional surgeries for glaucoma is a trabeculectomy. It can be used to treat closed-angle and open-angle glaucoma. During a trabeculectomy, the surgeon creates a small passage or flab in the white of the eye for fluid to drain. A small pocket is also created in the conjunctiva, which is called a bleb. The excess fluid drains out through the flab into the pocket. The aqueous fluid is then absorbed into the eye tissue, which decreases eye pressure. Another surgical option is a drainage tube insertion. During the procedure, a drainage device is surgically implanted into the eye. Although different drainage devices are available, they work the same. The surgeon also creates a reservoir, into which the drainage device directs the fluid, where it collects and is absorbed by the eye tissue. To learn more about conventional surgery and trabeculectomy for treatment of glaucoma, please visit our webpage, Surgical Treatment for Open Angle Glaucoma. Minimally Invasive Glaucoma Surgery (MIGS) If your ophthalmologist feels you are a candidate, he or she may recommend minimally invasive glaucoma surgery, or MIGS. Like conventional glaucoma surgery, the aim of MIGS is to reduce pressure in your eye, to prevent (further) damage to the optic nerve. However, it does so in a way that reduces potential complications associated with conventional glaucoma surgeries. When opting for MIGS, glaucoma surgeons use microscopic equipment and incisions to treat your eye. According to the Glaucoma Research Foundation, “While they reduce the incidence of complications, some degree of effectiveness is also traded for the increased safety.” There are four types of MIGS procedures that can be used to treat glaucoma, depending upon your particular condition:
Your eye surgeon will be able to discuss which, if any, of these procedures may be right for you. iStent Procedure for Glaucoma & Cataract Treatment If you should have glaucoma and cataracts, your eye surgeon may recommend the iStent procedure for you. Implanted during cataract surgery, the iStent is a tiny device that helps to decrease pressure in your eye, by restoring outflow of fluid from your eye. The benefit is having both conditions treated at once, if you are a candidate. If you have cataracts and glaucoma, you can ask your ophthalmologist if iStent may be a good option for you. Tips for Effective Glaucoma Treatment There are things you can do to increase the chances of successful treatment for glaucoma, including the following:
Even with these tips in mind, the most important steps you can take for your eyes are to understand your risk of glaucoma and get regular, comprehensive eye exams as directed by your eye doctor. Routine eye exams can allow your eye doctor to detect signs of glaucoma before you experience symptoms or any changes in vision. If you have any questions about glaucoma, your risk, your next eye exam, or glaucoma treatment and surgery or if you would like to schedule an eye exam with one of our ophthalmologists, please call our office at 508-746-8600. We hope you found valuable information in this post. Please check back soon. Comments are closed.
|
EYE HEALTH BLOGCategories
All
Archives
July 2024
|
|
Kadrmas Eye Care New England
55 Commerce Way, Plymouth, MA 02360
14 Tobey Road, Wareham, MA 02571 133 Falmouth Road (Rt 28), Mashpee, MA 02649 |
Phone Number:
1-508-746-8600 Hours: Monday through Friday — 8 AM – 4:30 PM |

 RSS Feed
RSS Feed
