|
March is National Save Your Vision Month, and in our five-part blog series, we’re taking a look at common causes of vision loss in adulthood, eye exams, general eye health, and signs telling you to have your eyes checked. In this second blog post, we explore common causes of vision loss in younger adults, both of which affect the retina:
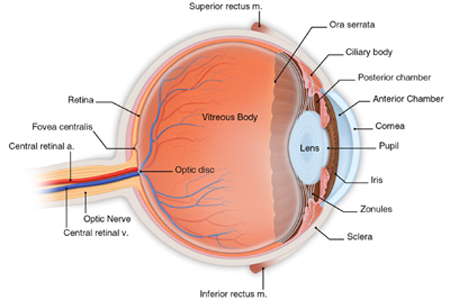
Retinal Tears & Detachments Retinal tears and detachments are optical emergencies that can cause blindness if not evaluated and treated promptly (within 24 hours). If you or a loved one experience any of the symptoms listed below, contact our office or your eye doctor immediately. Retinal tears and detachments happen as the vitreous gel, the fluid fills the eye and helps it maintain its shape, changes shape as we get older. It tends to shrink and pull away from the retina, the thin nerve layer at the back of the eye at that accepts light and transmits images to the brain via the optic nerve. In some cases, this shrinkage of the vitreous gel can cause the retina to tear or pull away from the back of the eye, usually in the peripheral (side) areas. When the retina tears or pulls away, fluid can leak through the retina and cause it to actually lift off the back of the eye. Once this process begins, it usually continues until most of or the entire retina has detached. If this happens, the light receptors in the retina will no longer be able to accept light or send images to the brain, which results in loss of vision. Fortunately, prompt treatment can repair tears in the retina and reattach the retina to the back of the eye, which is why it is so important to contact your eye doctor immediately if you or a loved one begin to experience any of the following symptoms or warning signs:
While these symptoms are warning signs, they do not always signify a retinal tear or detachment. However, due to the need to be evaluated and treated by an ophthalmologist who specializes in retinal tears and detachments promptly, don’t wait to call your eye doctor if you or a loved one develop any of these symptoms. Certain people, such as people who are middle age and older, are at a higher risk for retinal tears and detachments due to normal shrinkage of the vitreous gel. In addition, the following increase risk of developing this serious condition:
Your ophthalmologist can detect a retinal tear or detachment through a dilated eye examination, which allows the doctor to examine your retina using a device called an ophthalmoscope. This examination will help your eye doctor understand the severity of your condition and whether the macula, the area of the retina responsible for fine, detailed vision used for activities such as reading and writing, is involved. Further, it will help your eye surgeon understand whether laser or surgical treatment is right for your particular retinal tear or detachment. To learn more about retinal tears and detachments, as well as treatment options for these optical emergencies, visit our retinal tears and detachment webpages. Diabetic Retinopathy Diabetic retinopathy, caused by vascular changes in the retina (the light sensitive area in the back of the eye) related to diabetes, is one of the leading causes of vision loss and blindness in adults. In some cases, blood vessels in eye may swell and leak, whereas in other cases, abnormal new blood vessels may grow on the retina. Diabetic retinopathy occurs in four stages:
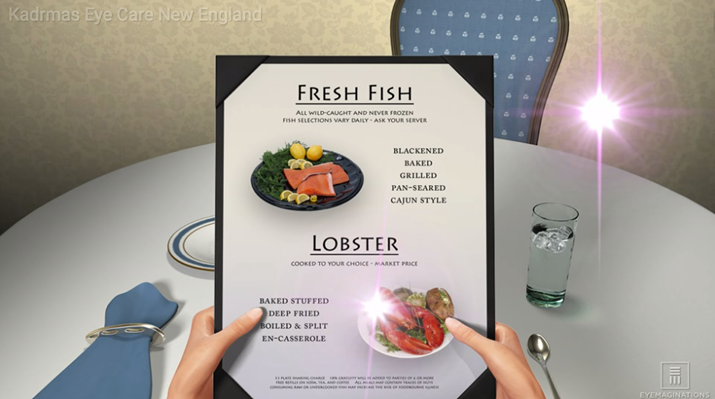
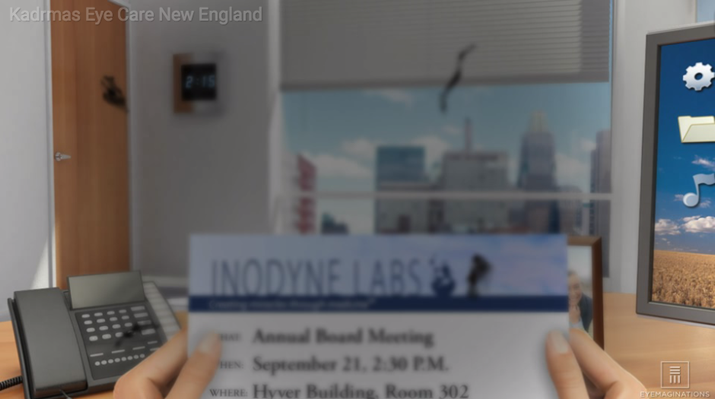
Vision loss can begin to occur at any stage of diabetic retinopathy. However, as the disease progresses and the macula is affected and bleeding worsens, many will notice vision changes in Stage 3 and blurry vision in Stage 4 diabetic retinopathy. If macular edema is present, fine vision used for reading, writing, and other detailed work may become diminished or lost. In addition to vision loss, black spots or flashes of light in central vision may become noticeable as diabetic retinopathy progresses. These can be symptoms of a detached retina or vitreous hemorrhage, both of which can cause a rapid loss of vision and constitute a medical emergency. If you notice any of these symptoms, you should see your ophthalmologist or eye doctor immediately. While it is not possible to restore lost vision, prompt treatment by your ophthalmologist who specializes in diabetic retinopathy can prevent further vision loss. Everyone with diabetes is at risk for diabetic retinopathy, regardless of the type. However, people who have had diabetes for longer are at greater risk. If you have diabetes, you should have a dilated eye exam once a year. Because proliferative retinopathy and macular edema can occur without noticeable vision loss, your vision may be at risk without regular examination, and early detection and treatment of diabetic retinopathy can prevent vision loss. If you are pregnant and have diabetes, you should see your eye doctor as soon as possible, as more frequent eye examinations to check for signs of diabetic retinopathy may be needed. If you have been diagnosed with diabetic retinopathy, you may also need dilated eye exams more frequently. In addition to dilated eye exams, your eye doctor will perform a comprehensive eye examination to diagnose and monitor diabetic retinopathy, including: These tests will help your ophthalmologist understand your condition and determine the best course of treatment for you. To learn more about diabetic retinopathy and medical, laser, therapeutic injection, and surgical treatments for this condition, please visit our diabetic eye disease webpages. Specialists in Retinal Tears, Retinal Detachments & Diabetic Retinopathy If you or a loved one is suffering from or has symptoms consistent with either of these conditions described above, please contact us. Our ophthalmologists, who specialize in these conditions as listed below, are here to help save your vision:
Comments are closed.
|
EYE HEALTH BLOGCategories
All
Archives
July 2024
|
|
Kadrmas Eye Care New England
55 Commerce Way, Plymouth, MA 02360
14 Tobey Road, Wareham, MA 02571 133 Falmouth Road (Rt 28), Mashpee, MA 02649 |
Phone Number:
1-508-746-8600 Hours: Monday through Friday — 8 AM – 4:30 PM |

 RSS Feed
RSS Feed
